I regularly scan research output from disciplines other than economics that I think impacts on economic matters. On April 17, 2024, a new study from medical researchers at the Burnett Institute in Melbourne, working with staff at the Department of Health and Human Services, in Victoria published a pre-print in The Lancet – Admission Screening Testing of Patients and Staff N95 Masks are Cost-Effective in Reducing COVID-19 Hospital Acquired Infections – which continues to show that public health policy in Australia is failing and part of that failure is the myopia that ‘sound finance’ principles engenders. I have written before about this myopia where governments think they need to cut back on spending because they are ‘short’ of funding and end up having to spend more over time because the initial spending cuts cause massive (and predictable) problems. We have seen this phenomenon in many situations (several cases are cited below). This new research puts an end in my view to the debates about hospital and more general health practices in the Covid era and exposes how the lack of political leadership, a refusal to fund public education, and poor hospital practices – mostly due to alleged funding shortfalls – have turned Australian hospitals into death zones. And while the authorities are telling the public they are ‘saving taxpayers’ money’ the reality is that the pubic outlays to deal with the problems they are creating by this austerity will be multiples of what would be required to implement sound policy now and avoid those longer-term problems.
There are countless examples now of this type of neoliberal myopia and I have covered them in these blog posts (among others) over many years of study:
1. More privatisation myopia (March 22, 2021) – privatisation of world-leading vaccine producer in Australia.
2. Neoliberal myopia strikes again (December 16, 2020) – long-term impacts of cuts in health infrastructure.
3. Mental illness and homelessness – fiscal myopia strikes again (January 5, 2016) – housing and homelessness.
4. British floods demonstrate the myopia of fiscal austerity (January 4, 2016) – British flooding
5. The myopia of fiscal austerity (June 10, 2015) – British canal rat infestation and collapse of Manchester sewers.
6. The myopia of neo-liberalism and the IMF is now evident to all (October 8, 2014) – long-term income losses from austerity.
7. Myopic meanness – Australia’s ODA cuts to its neighbours in the Pacific (April 5, 2022) – loss of strategic geopolitical position due to cuts to foreign aid.
8. Australia’s bushfire dystopia – another entry for the neoliberal report card (January 9, 2020) – refusal to fund climate transition and bushfire damage.
The research paper I cited in the introduction comes from the – Burnett Institute – which is a world-leading medical research group that “combines medical research in the laboratory and the field, with public health action to address major health issues affecting disadvantaged communities in Australia, and internationally.”
It specialises in infectious disease research and helps design public health programs in Australia, Africa, Oceania and Asia.
It provided early and leading research in the study of HIV, influenza and STDs.
In this latest research, we learn that previous claims that N95 mask-wearing makes no different to the spread of Covid especially in hospital settings, which have been weaponised by policy makers intent on ‘saving’ health expenditure, do not stack up.
The research was motivated by the on-going debate about how to deal with life-threatening infections in health care settings.
That is, a person enters a hospital for a routine operation expecting to come out soon enough after surgery, but, instead catches Covid, becomes very ill, and dies in the hospital.
That type of phenomena is rising in incidence although authorities are reluctant to publish the (embarrassing data).
A dear friend of mine lost his long-time partner recently after she was hospitalised after a fall but acquired Covid in the hospital and never came out.
A UK study found that “11.3% of hospitalised COVID-19 patients acquired COVID-19 whilst in hospital …, 11.8% in Germany … and 9.2% in Brazil …”
Between 2020 and 2022, Australian hospital workers were required to observe strict protocols to reduce these types of infections.
However, under pressure from the vocal anti-vax, freedom lobby combined with an obsessive quest for a fiscal surplus (to ‘save’ money) the Australian government relaxed all the pandemic orders in 2023 and left it up to individual entities to implement whatever infection control and prevention protocols they liked.
And the funding was severely cut, which placed pressures on the health care providers (hospitals, clinics etc) to reduce the procedures to, in some cases, nothing!
The results have been obvious – “many acute care settings have ceased testing patients on admission” and abandoned the use of N95 masks all while COVID-19:
… continues to cause epidemic transmission and impacts.
Within this context, the Burnett researchers noted that:
… there is limited understanding of the most cost-effective ways to reduce infections, in particular COVID-19 hospital-acquired infections.
They sought to quantify:
… the cost benefits of different patient testing and mask types in acute care facilities, as well as evaluating and comparing the efficacy of these interventions applied continually versus only during periods of high COVID-19 prevalence.
They deployed an ‘agent-based model’ calibrated with real world health data to simulate different cost trajectories and then analysed these trajectories by “comparing different configurations of patient admission screening testing and staff mask usage”.
I won’t elaborate on their research techniques but they are sound.
They modelled three different types of interactions within acute wards – “patient-patient, staff-staff, and staff patient”.
They didn’t model visitor impacts but suggest that their outcomes are understated because of this.
They modelled different testing protocols – PCR and RATs as well as the use of N95 masks as opposed to the less protective surgical masks.
Data was supplied by the Victorian Health Department.
Taken together they then calculated different health outcome scenarios (excluding Long Covid cases – which means they again understate the severity) and then applied input data to each simulated scenario to assess the total costs of each in 2023 $A terms.
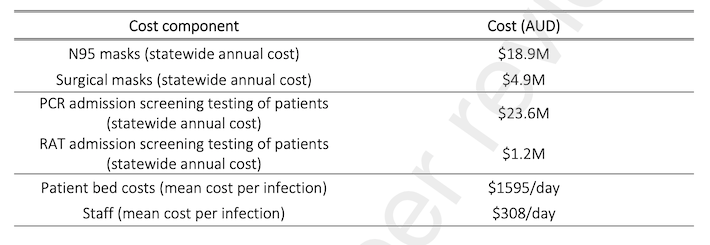
The cost inputs were interesting and represented by this Table.
It is obvious that massive savings to government arise from scrapping any mandates to wear N95 masks and to screen for Covid on admission.
You can also see the cost of each infection per day.
What becomes obvious from the study is that quite apart from the health risks of Covid, including the high death rate and the increasing probability of ending up with Long Covid and all the other complications to hearts, brains, livers etc – the bean counters have got the basic calculations wrong.
This graph summarises the scenarios and the relative total costs.
The results of the study are:
1. “Compared to a reference of no admission screening testing of patients and staff surgical masks, all scenarios were cost saving with health gains over a 12-month period”.
2. “the testing or N95 costs were small in comparison to the cost of additional patient bed days due to hospital-acquired infections.”
3. “Staff N95s were cost saving with health gains compared to surgical masks regardless of admission screening …”
4. “PCR admission screening and N95 usage shows the most QALYs gained” – QALYs = total-quality-adjusted life years.
The researchers conclude that while the use of N95 masks and tight admission testing procedures deliver the best health and cost outcomes:
One of the reasons that staff N95 masks and patient admission screening testing have been removed … is the high upfront costs in a context where emergency pandemic funding was removed.
They also argue that with no restrictions in place within the community, more people are checking into hospital for whatever reason who are infected with Covid.
With the lax protocols in place once they are admitted – no special wards etc – they quickly spread the infections to fellow patients and medical staff (who are not using N95 masks), who, in turn, spread the disease more widely both throughout the acute care facility but also back into the community.
Their overall conclusion is that:
… N95 mask use and admission screening testing of patients can save lives and reduce costs related to COVID-19 through reduced patient bed days and staff replacement needs. The more they can practically be implemented the greater the impact is likely to be. Infection prevention and control measures to reduce COVID-19 transmission in acute care settings should continue to be applied.
A definitive conclusion.
The message is clear: trying to ‘save’ outlays by compromising the quality and scope of public infrastructure and services ends up ‘costing’ more over time.
The bean counters celebrate in the short-run their cleverness in cutting ‘costs’ and are mute when the reality dawns that they are actually mindlessly stupid.
And in this particular context – where unnecessary Covid deaths are rising in the hospitals because they have become enclosed infection breeders – the stupidity is in my view criminal.
This ABC news report (May 6, 2024) – Hundreds of patients died after catching COVID in Victorian hospitals, new data shows – summarises the latest available data, which is becoming increasingly difficult to obtain.
Scrutiny of the policy process on this issue is getting difficult because the governments (federal and state) are deliberately suppressing data or abandoning the collection of it.
The Report notes that:
For months doctors and public health experts have been warning that too many patients are catching COVID in Australian hospitals with sometimes devastating consequences — though timely statistics are difficult to access because health departments do not publish them …
Alarmingly, the proportion of hospitalised COVID patients who caught the virus in public hospitals was much higher last year than in 2022 — up from 13 per cent to 20 per cent, on average — coinciding with a reduction in COVID screening and healthcare worker mask use across the state.
In 2023, for example, 2,322 patients contracted Covid from the hospital and more 9 per cent died.
The Report notes that in some cases, people have been admitted to hospital for routine procedures, then become infected with Covid, which, in turn, triggered neurological illness (Huntington’s Disease in the case cited).
N95 mask wearing among the staff was absent in the case cited.
The current research is pointing to the fact that:
The numbers indicate that there is a big problem here — these infections and deaths are potentially preventable
I cannot imagine why we would tolerate that – it is sort of back to the dark ages of ignorance and indifference.
The ABC Report offers some clues.
1. Senior hospital executives think Covid “is just a cold” – they are political appointments and do the work of the bean counters in government.
2. People claim they are “tired of wearing masks” – so why are they not tired of wearing belts or shoes or anything really.
I wear a mask in every setting where there is a risk of infection.
I have grown used to it and it is now routine.
The benefits of not getting sick vastly outweigh the minor inconvenience of wearing the protection.
The fact that the population doesn’t see that reflects the lack of education provided by the government on this issue.
If the general public was apprised of the latest research and its implications for their long-term health then things might change a bit.
And if there was more collective will or solidarity engendered rather than the promotion of rampant individualism then things might change a bit.
There is a reason the Japanese people are high mask wearers – there is a culture of respect and concern for one’s impact on others, that has disappeared in other nations that have been assaulted by neoliberalism.
One hospital that the ABC Report investigated – the Royal Melbourne – has maintained strict testing and mask wearing protocols as well as providing advanced air ventilations technologies and considers – “any sort of nosociomial infection is a disaster”.
So if you ever need to go to a hospital in Victoria try to get in there!
Conclusion
We have been assaulted with federal and state government campaigns against smoking for years.
Road safety campaigns are always prominent and there are advertisements regularly in the media.
Why then has the government gone silent and passive on Covid?
The pandemic is still killing thousands and crippling more.
Our acute care facilities are no longer safe to enter for care.
The risk of becoming infected with Covid and dying in one of these facilities as a consequence is significant and rising.
The policy neglect is actually ‘costing’ government more over time than the short-term cost reductions that accompanied the relaxation of the protocols.
Why then is there policy neglect?
That is enough for today!
(c) Copyright 2024 William Mitchell. All Rights Reserved.